Ways to recognize Stroke early

The F.A.S.T (Face, Arms, Speech and Time) algorithm is a quick method of assessing whether a person might be experiencing a stroke and is a strong reminder that stroke is an emergency.
Stroke is an emergency:
After a stroke, acute treatment to minimise the severity of the outcome, rehabilitation to recover any lost function and prevention of recurrence are of great importance.
Time is brain:
Following a stroke, approximately 1.9 million neurons are lost every minute in the ischemic area if left untreated. Loss of brain tissue means loss of function and long-term disability or death. It is therefore imperative that a stroke is recognised early, the stroke patient is taken directly to a stroke unit (preferably using an established stroke network), and diagnosis and treatment follow as quickly and efficiently as possible.
Pathophysiology
(How does a Stroke occur?)
A stroke occurs when the blood flow to an area of the brain is interrupted, resulting in some degree of permanent neurological damage. The two major categories of stroke are ischaemic (lack of blood and hence oxygen to an area of the brain) and haemorrhagic (bleeding from a burst or leaking blood vessel in the brain) stroke.
Pathophysiology of ischemic stroke
The common pathway of ischemic stroke is lack of sufficient blood flow to perfuse cerebral tissue, due to narrowed or blocked arteries leading to or within the brain.
Ischemic strokes can be broadly subsided into thrombotic and embolic strokes.
Narrowing is commonly the result of atherosclerosis – the occurrence of fatty plaques lining the blood vessels. As the plaques grow in size, the blood vessel becomes narrowed and the blood flow to the area beyond is reduced. Damaged areas of an atherosclerotic plaque can cause a blood clot to form, which blocks the blood vessel – a thrombotic stroke. In an embolic stroke, blood clots or debris from elsewhere in the body, typically the heart valves, travel through the circulatory system and block narrower blood vessels.
Based on the aetiology of ischemic stroke, a more accurate sub-classification is generally used:
Large artery disease– atherosclerosis of large vessels, including the internal carotid artery, vertebral artery, basilar artery, and other major branches of the Circle of Willis.
Small vessel disease – changes due to chronic disease, such as diabetes, hypertension, hyperlipidaemia, and smoking that lead decreased compliance of the arterial walls and/or narrowing and occlusion of the lumen of smaller vessels.
Embolic stroke – the most common cause of an embolic stroke is atria fibrillation.
Stroke of determined aetiology – such as inherited diseases, metabolic disorders, and coagulopathies.
Stroke of undetermined aetiology – after exclusion of all of the above.
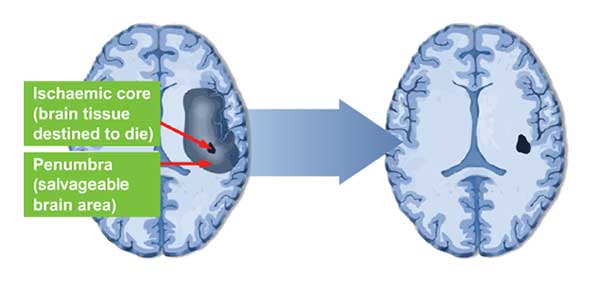
In the core area of a stroke, blood flow is so drastically reduced that cells usually cannot recover and subsequently undergo cellular death.
The tissue in the region bordering the infarct core, known as the ischemic penumbra, is less severely affected. This region is rendered functionally silent by reduced blood flow but remains metabolically active. Cells in this area are endangered but not yet irreversibly damaged. They may undergo self destruction after several hours or days but if blood flow and oxygen delivery is restored shortly after the onset of stroke, they are potentially recoverable.
Ischemic penumbra – Potential to reverse neurologic impairment with post-stroke therapy .
Pathophysiology of haemorrhagic stroke:
Haemorrhagic strokes are due to the rupture of a blood vessels leading to compression of brain tissue from an expanding haematoma. This can distort and injure tissue. In addition, the pressure may lead to a loss of blood supply to affected tissue with resulting infarction, and the blood released by brain haemorrhage appears to have direct toxic effects on brain tissue and vasculature.
Intra-cerebral haemorrhage– Caused by rupture of a blood vessel and accumulation of blood within the brain. This is commonly the result of blood vessel damage from chronic hypertension, vascular malformations, or the use medications associated with increased bleeding rates, such as anticoagulants, thrombolytics, and anti-platelet agents.
Subarachnoid haemorrhage is the gradual collection of blood in the subarachnoid space of the brain dura, typically caused by trauma to the head or rupture of a cerebral aneurysm.